Benefits of prior authorization by IMBS
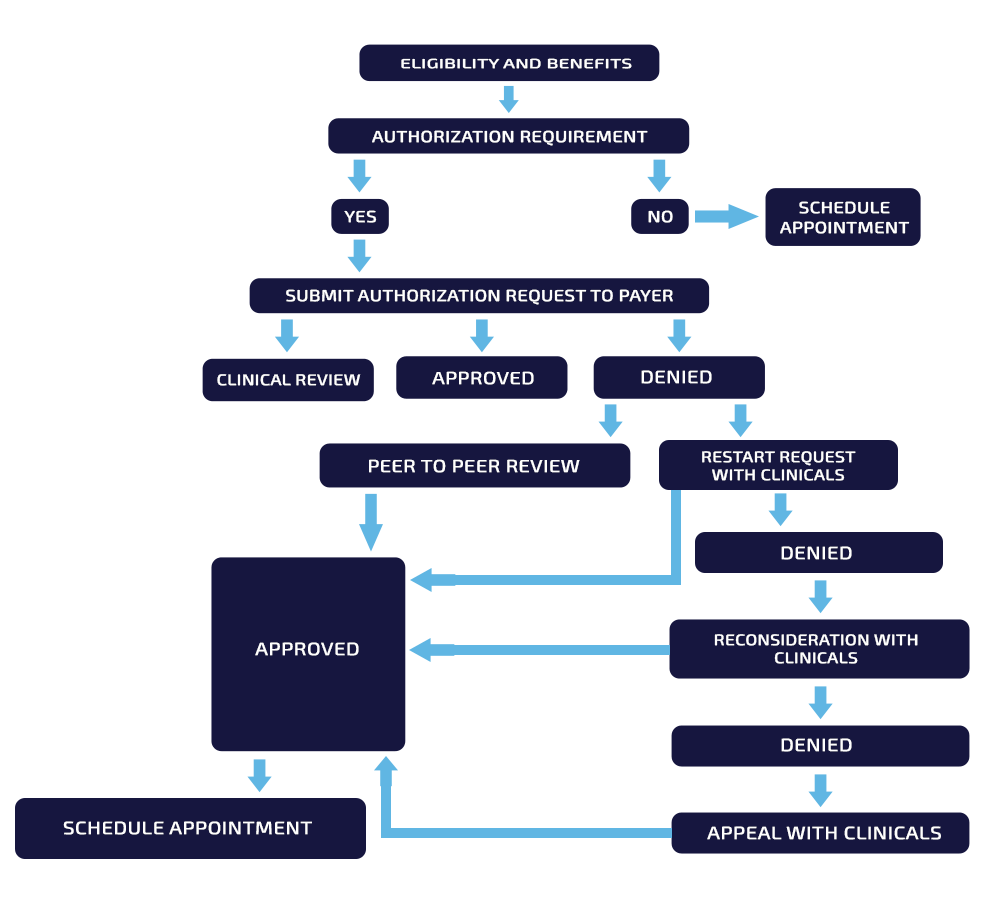
Prior authorization (also called pre-certification) is the process where certain medical services, tests, or procedures require approval from an insurance company before treatment is provided. This ensures that the proposed care is medically necessary and aligns with payer requirements.
Not all procedures require prior authorization—each insurance company maintains a list of services that need approval. After reviewing the treatment plan submitted by the provider, the insurance company’s Utilization Management (UM) or Medical Review department grants the authorization. Emergency cases are generally exempt from this process.
Prior Authorization Workflow Process :
Importance of Authorization :
IMBS expert team proactively initiates the prior authorization process at least 15 days prior to appointments, ensuring timely approval of medical necessity treatments and minimizing the risk of treatment delays or re-scheduling. In addition, The Prior Authorization method improves revenue and allows appropriate reimbursement for healthcare services.
Authorization does not guarantee payment; however, if the claim is denied, we can file an appeal with the authorization number to seek reimbursement from the insurance carrier. Lack of authorization might result in costly consequences for both the patient and the healthcare practitioner. Therefore, having a partner like IMBS handle your medical billing and authorization procedure is the key to higher reimbursement.